Doctors Refuse CPR On College Student: The Shocking Truth And What You Need To Know
Imagine this: A young college student collapses on campus, and instead of receiving immediate life-saving care, doctors refuse to perform CPR. Sounds like something out of a nightmare, right? But unfortunately, it's a reality that has sparked heated debates in the medical world. Doctors refusing CPR on college students is not just a medical issue—it's a moral, ethical, and legal dilemma that affects us all.
Let's dive into the heart of the matter. When we think about college life, we imagine late-night study sessions, parties, and the thrill of independence. But what happens when that independence is suddenly cut short because of a medical emergency—and the very people who are supposed to save lives choose not to act? It's a scenario that leaves many of us scratching our heads and wondering, "How could this happen?"
Now, before we jump into the nitty-gritty, let's be clear: this article isn't here to point fingers or stir up drama. Instead, it's designed to shed light on a critical issue that affects students, parents, and medical professionals alike. So, buckle up because we're about to break it down in a way that's both informative and easy to digest.
Read also:Baddies East Sky The Ultimate Guide To Understanding The Phenomenon
Table of Contents
- What Happens When Doctors Refuse CPR?
- Why Do Doctors Refuse CPR on College Students?
- The Legal and Ethical Implications
- Understanding DNR Orders
- How Common Is This Issue?
- What Can Students Do to Protect Themselves?
- The Role of Medical Institutions
- Case Studies: Real-Life Examples
- What Parents Need to Know
- Final Thoughts and Next Steps
What Happens When Doctors Refuse CPR?
Let's start with the basics. When doctors refuse to perform CPR, it can mean life or death for the patient involved. CPR, or cardiopulmonary resuscitation, is a life-saving technique used to restore blood flow and oxygen to the heart and brain when someone's heart stops beating. It's one of the first lines of defense in emergency situations, and its importance cannot be overstated.
But what happens when medical professionals decide against performing CPR? In some cases, it leads to irreversible brain damage or even death. The consequences are devastating, not just for the student but also for their family and friends. This is why understanding the reasons behind such decisions is crucial.
Here's the kicker: there are situations where CPR might not be the best option, and we'll dive deeper into that later. But for now, let's focus on the fact that these decisions have far-reaching implications that go beyond the individual case.
Why Is CPR Important in Emergencies?
CPR is more than just a medical procedure—it's a lifeline. Without it, the chances of survival drop significantly within minutes. For college students, who are often far from home and may not have immediate access to family or support systems, the role of medical professionals becomes even more critical.
Why Do Doctors Refuse CPR on College Students?
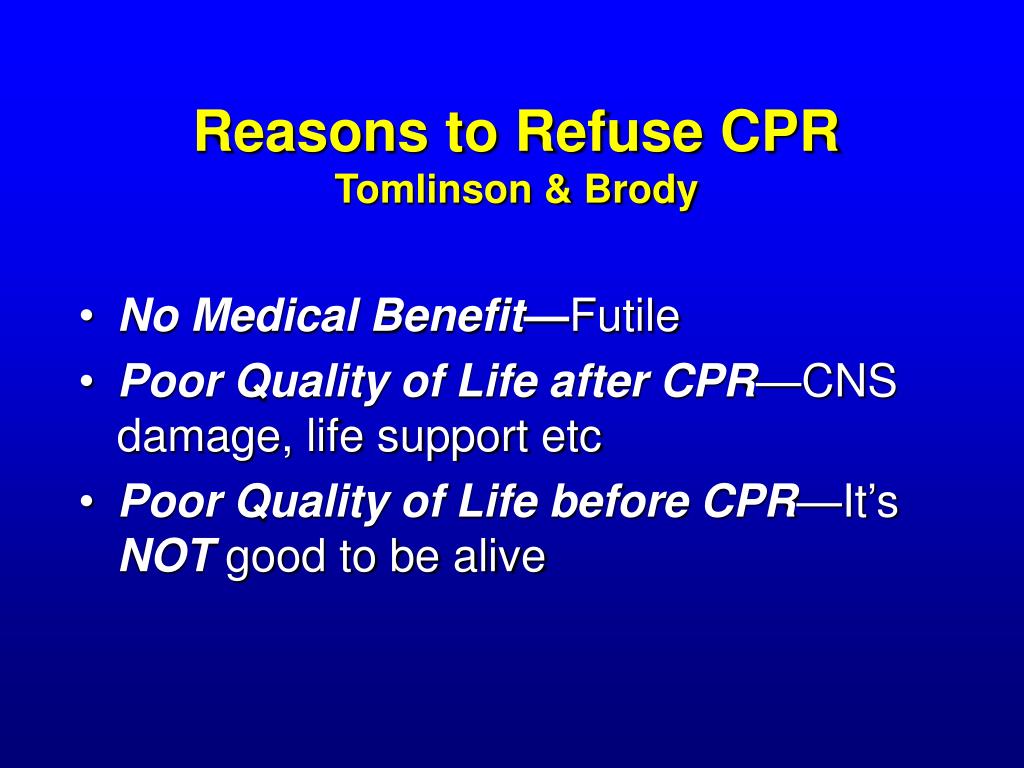
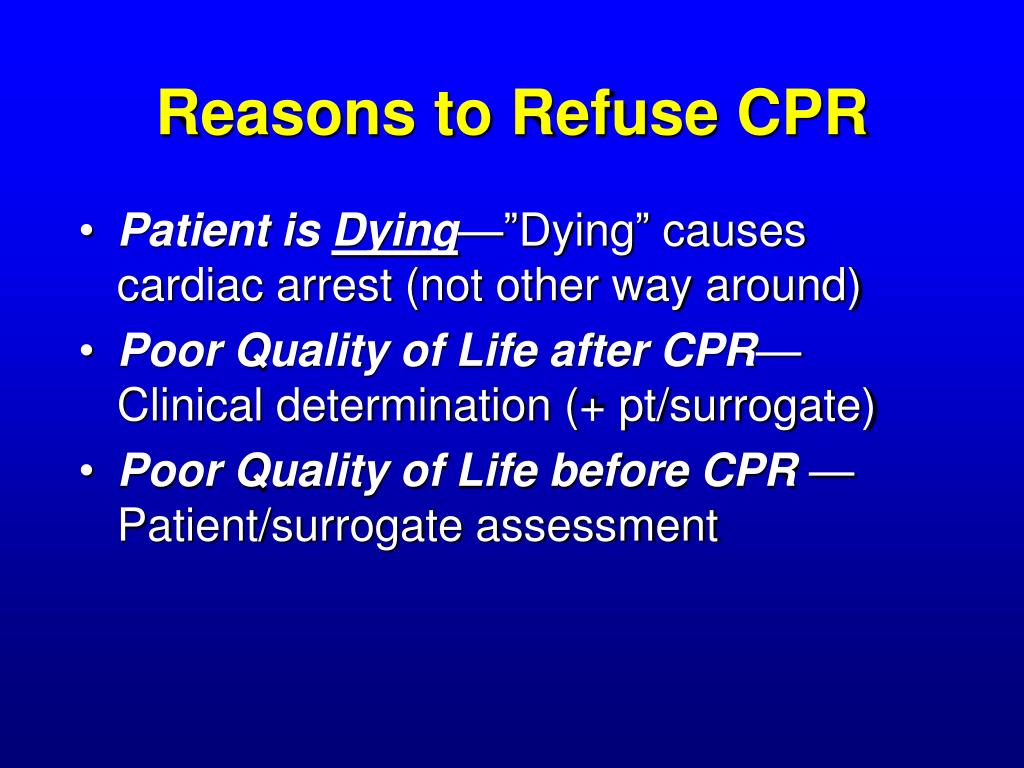
Now, here's the part where things get a little complicated. There are several reasons why doctors might refuse to perform CPR on college students. Some of these reasons are rooted in medical ethics, while others are tied to legal considerations or personal beliefs. Let's break it down:
- Do Not Resuscitate (DNR) Orders: In some cases, the patient may have a DNR order in place, which explicitly states that they do not want to be resuscitated in the event of a cardiac arrest.
- Futility of Treatment: If the patient's condition is deemed terminal or irreversible, doctors may decide that CPR would not be beneficial and could even cause more harm than good.
- Legal Concerns: Medical professionals sometimes fear legal repercussions if something goes wrong during CPR, leading them to err on the side of caution.
- Personal Beliefs: Believe it or not, some doctors may have personal beliefs or biases that influence their decision-making process.
It's important to note that these reasons don't always align with the patient's wishes or best interests. That's why open communication and clear documentation are essential in these situations.
Read also:Julio Immigration Lawyer Your Trusted Ally In Navigating Complex Legal Waters
The Legal and Ethical Implications
When doctors refuse CPR, they're not just making a medical decision—they're also navigating a minefield of legal and ethical considerations. On one hand, they have a duty to act in the best interest of their patients. On the other hand, they must adhere to legal guidelines and respect the patient's autonomy.
Here's the thing: the law varies from state to state and country to country. In some places, doctors are legally obligated to perform CPR unless there's a valid DNR order. In others, they have more discretion. This inconsistency can lead to confusion and, in some cases, tragedy.
Ethically speaking, refusing CPR can raise questions about the doctor's commitment to their Hippocratic Oath. After all, "do no harm" is a guiding principle in medicine. But what constitutes harm? Is it causing physical pain during CPR, or is it allowing someone to die without trying to save them?
How Do Legal Systems Address This Issue?
Legal frameworks around CPR refusal are complex and often open to interpretation. For instance, in the United States, the Emergency Medical Treatment and Active Labor Act (EMTALA) requires hospitals to provide stabilizing treatment to anyone who comes to the emergency department, regardless of their ability to pay. However, this doesn't always cover situations where CPR is deemed unnecessary or harmful.
Understanding DNR Orders
One of the most common reasons doctors refuse CPR is the presence of a DNR order. A DNR, or Do Not Resuscitate order, is a legal document that instructs medical personnel not to perform CPR in the event of cardiac arrest. It's often used by patients with terminal illnesses or those who prefer to die naturally without medical intervention.
But here's the catch: not all college students are aware of DNR orders or their implications. Many may not have had the conversation with their families or doctors about end-of-life care. This lack of awareness can lead to misunderstandings and missed opportunities for clarity.
For example, a student might collapse on campus, and the medical team assumes there's a DNR order in place when there isn't. Or worse, they might honor a DNR order that the student didn't fully understand or agree with. These scenarios highlight the importance of education and communication.
How Can Students Create a DNR Order?
Creating a DNR order is a straightforward process, but it requires careful consideration. Students should discuss their wishes with their families and healthcare providers and ensure that the order is properly documented and accessible in case of an emergency. It's also important to review and update the order as circumstances change.
How Common Is This Issue?
You might be wondering how often doctors actually refuse CPR on college students. While exact statistics are hard to come by, anecdotal evidence suggests that it's more common than we'd like to believe. College campuses are unique environments where students are often away from their usual healthcare providers, making it harder to access critical medical information.
According to a study published in the Journal of Medical Ethics, about 10% of medical professionals surveyed admitted to refusing CPR in certain situations. While this percentage may seem small, it represents a significant number of potential lives lost.
Furthermore, the lack of standardized protocols across medical institutions means that some students may receive life-saving care while others do not, depending on where they happen to be when an emergency occurs.
What Are the Statistics Saying?
Data from the American Heart Association shows that immediate CPR can double or even triple a person's chances of survival after cardiac arrest. However, only about 46% of people who experience cardiac arrest outside of a hospital receive bystander CPR. These numbers underscore the importance of education and preparedness in emergency situations.
What Can Students Do to Protect Themselves?
So, what can college students do to ensure they receive the care they need in an emergency? Here are a few tips:
- Have the Conversation: Talk to your family and healthcare providers about your wishes regarding CPR and other life-saving measures.
- Carry a Medical ID: Wear a medical alert bracelet or carry a card in your wallet that lists your medical conditions, allergies, and any DNR orders.
- Know Your Rights: Familiarize yourself with the laws and policies regarding CPR in your state or country.
- Learn CPR: Take a CPR course so you can help others in need and advocate for yourself if necessary.
By taking these proactive steps, students can empower themselves and reduce the likelihood of misunderstandings or miscommunication in emergency situations.
The Role of Medical Institutions
Medical institutions also play a critical role in addressing this issue. They need to establish clear policies and protocols for handling CPR refusals and ensure that all staff members are trained to follow them consistently. Additionally, they should prioritize education and awareness campaigns to inform students and their families about their rights and options.
One way to achieve this is by partnering with local universities and community organizations to provide workshops and resources on emergency preparedness. By fostering a culture of transparency and collaboration, medical institutions can help bridge the gap between patients and providers.
How Can Institutions Improve Communication?
Improving communication starts with building trust. Institutions can achieve this by being open and honest about their policies and procedures and by actively seeking feedback from patients and their families. Regular training sessions and refresher courses for staff members can also help ensure that everyone is on the same page.
Case Studies: Real-Life Examples
To better understand the impact of CPR refusals, let's look at a few real-life examples:
- Case 1: A 19-year-old college student collapses during a basketball game. Despite being surrounded by trained medical personnel, no one performs CPR because they mistakenly believe there's a DNR order in place. The student dies as a result.
- Case 2: A 22-year-old student with a known heart condition collapses in her dorm room. Her roommate performs CPR until paramedics arrive, saving her life. This highlights the importance of bystander CPR in emergency situations.
- Case 3: A 20-year-old student is refused CPR because the medical team deems it futile due to his underlying health conditions. His family sues the hospital, leading to a legal battle that raises important questions about medical ethics and accountability.
These cases illustrate the complexity and urgency of addressing CPR refusals in college settings.
What Parents Need to Know
Parents play a vital role in ensuring their children are prepared for medical emergencies. They should have open and honest conversations with their kids about CPR, DNR orders, and other life-saving measures. Additionally, they should encourage their children to carry medical IDs and learn basic first aid skills.
Parents can also advocate for better policies and resources at their children's universities by working with student organizations and campus health services. By staying informed and engaged, they can help create a safer and more supportive environment for all students.
How Can Parents Support Their Children?
Support starts with education. Parents should equip themselves with knowledge about CPR, DNR orders, and other medical procedures. They should also stay in touch with their children and encourage them to share any concerns or questions they may have about their health.
Final Thoughts and Next Steps
In conclusion, the issue of doctors refusing CPR on college students is a complex and multifaceted one that requires attention from all stakeholders. By understanding the reasons behind these decisions and taking proactive steps to address them, we can work towards a future where every student has access to the care they need in an emergency.
So, what can you do next? Start by having those tough conversations with your loved ones. Encourage them to learn CPR and carry medical IDs. And don't be afraid to advocate for change in your community and beyond. Together, we can make a difference.
And hey, don't forget to share this article with your friends and family. The more people who are aware of this issue, the better equipped we'll be to tackle it head-on. Because at the end of the day, it's all about saving lives—and that's something we can all get behind.